Our Surgical Procedures
Other Lasers
Laser Retinopexy for Retinal Tears
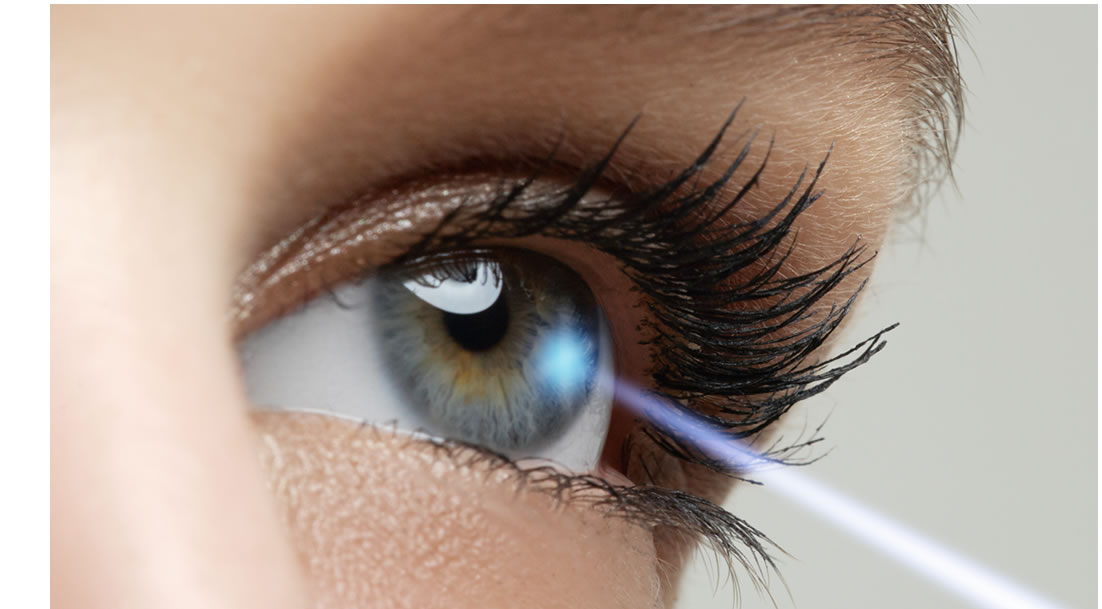
A retinal tear is a break in the retinal layer of the back of the eye. Only a small percentage of eyes have a retinal tear, and they can occur for a variety of reasons. Sometimes a tear can lead to a detachment, which is when the retina is pulled away from its normal position. This can occur because the fluid or jelly (vitreous) on the inside of the eye passes through the break, lifting the retina off the back of the eye, just like wallpaper can peel off a wall. A detachment is a very serious problem which can lead to blindness. Some retinal tears should be treated and others are such low risk that they can be followed with routine exams. One way to treat a retinal tear is to use an argon laser to seal the retina to the back wall of the eye. This is called a laser retinopexy, and is performed in an attempt to prevent a detachment. The laser is done in the office and usually causes only mild discomfort.
YAG Capsulotomy and Cataract Surgery
The most common side effect after cataract surgery is a posterior lens capsule opacification (PCO). This PCO is a hazy membrane which forms just behind the intraocular lens that was placed during surgery, and causes vision to be blurry. The hazy membrane can occur months or years after cataract surgery. A YAG laser treats this PCO effectively and painlessly in the office. No incisions are made. The laser takes only a few minutes, and there are no restrictions after the treatment. Sometimes, the ophthalmologist will recommend that an anti-inflammatory drop be used after the laser for a few days. Vision is often improved within one day. In general, the YAG capsulotomy is extremely safe. However there is a very slight increased risk of damage to the lens implant, retinal detachment, lens dislocation, retinal swelling, or transient elevation of eye pressure.
Lasers for Diabetes and Glaucoma
Laser for diabetes is often recommended for PDR, macular edema, and neovascular glaucoma. An argon laser is used in the office to shrink abnormal blood vessels. For PDR and neovascular glaucoma, the laser is focused on all parts of the retina except the macula, and is called panretinal photocoagulation treatment (PRP). PRP may decrease peripheral vision, but it is often effective in preserving the rest of the patient’s vision and in stopping the progression of disease. Other side effects can include decreased night vision, color vision or central vision. Laser does not cure diabetic retinopathy and does not always prevent further vision loss. For macular edema, the two common laser treatments are ‘focal laser’ and ‘grid laser’. The argon laser is focused in the macula with very low power. If you are diabetic and have any changes in your vision, please call us immediately to meet with one of our Board Certified Opthalmologists.
|
Prepare for Your Visit
For information regarding what to bring to your appointment, please visit our Patient Registration page.
Insurance and Payment
For important information regarding insurance and payment for your upcoming appointment and related insurance regulations, please visit our Insurance Information page.
Please Note: If you have a Vision Care benefit, your insurance provider may require the contact lens exam be performed on the same day as the vision exam. |
Diabetic Eye Exams
 Diabetes is an extremely common condition, and changes in the eyes are one of its most frequent complications. Since symptoms may not arise until very late in the disease process, yearly dilated diabetic eye exams by an ophthalmologist are strongly recommended. High blood sugar levels can damage blood vessels in the retina, the layer at the back of the eye that senses light and helps to send images to the brain. The damage to retinal vessels is referred to as diabetic retinopathy. This process takes place over time through many stages, and unfortunately can lead to a significant decrease in vision or even blindness. Diabetes is the leading cause of blindness in people ages 20-65. Diabetes is an extremely common condition, and changes in the eyes are one of its most frequent complications. Since symptoms may not arise until very late in the disease process, yearly dilated diabetic eye exams by an ophthalmologist are strongly recommended. High blood sugar levels can damage blood vessels in the retina, the layer at the back of the eye that senses light and helps to send images to the brain. The damage to retinal vessels is referred to as diabetic retinopathy. This process takes place over time through many stages, and unfortunately can lead to a significant decrease in vision or even blindness. Diabetes is the leading cause of blindness in people ages 20-65.
|
Diabetic Retinopathy
The early stage of diabetic retinopathy is called nonproliferative diabetic retinopathy (NPDR). In this stage, tiny blood vessels within the retina leak blood or fluid. The leaking fluid causes the retina to swell or to form deposits called exudates. A later stage of diabetic retinopathy is called proliferative diabetic retinopathy (PDR). PDR is present when abnormal new vessels (neovascularization) begin growing on the surface of the retina or optic nerve. Unfortunately these new blood vessels do not work well, and can cause further leaking, bleeding, or decreased vision. The macula is a small region in the center of the retina that allows us to see fine details clearly. In diabetic retinopathy, macular thickening or swelling can occur, called macular edema. Occasionally, new blood vessels can even grow on the iris (the colored part of the eye) and block the normal flow of fluid out of the eye. Pressure in the eye can build up, causing neovascular glaucoma, a severe eye disease which causes damage to the optic nerve. |
|
Like us on  |




 Diabetes is an extremely common condition, and changes in the eyes are one of its most frequent complications. Since symptoms may not arise until very late in the disease process, yearly dilated diabetic eye exams by an ophthalmologist are strongly recommended. High blood sugar levels can damage blood vessels in the retina, the layer at the back of the eye that senses light and helps to send images to the brain. The damage to retinal vessels is referred to as diabetic retinopathy. This process takes place over time through many stages, and unfortunately can lead to a significant decrease in vision or even blindness. Diabetes is the leading cause of blindness in people ages 20-65.
Diabetes is an extremely common condition, and changes in the eyes are one of its most frequent complications. Since symptoms may not arise until very late in the disease process, yearly dilated diabetic eye exams by an ophthalmologist are strongly recommended. High blood sugar levels can damage blood vessels in the retina, the layer at the back of the eye that senses light and helps to send images to the brain. The damage to retinal vessels is referred to as diabetic retinopathy. This process takes place over time through many stages, and unfortunately can lead to a significant decrease in vision or even blindness. Diabetes is the leading cause of blindness in people ages 20-65.